The IUD is one of the most effective forms of birth control available, with less than 1% failure rate. It is an attractive birth control, especially for women who are concerned taking a pill every day.
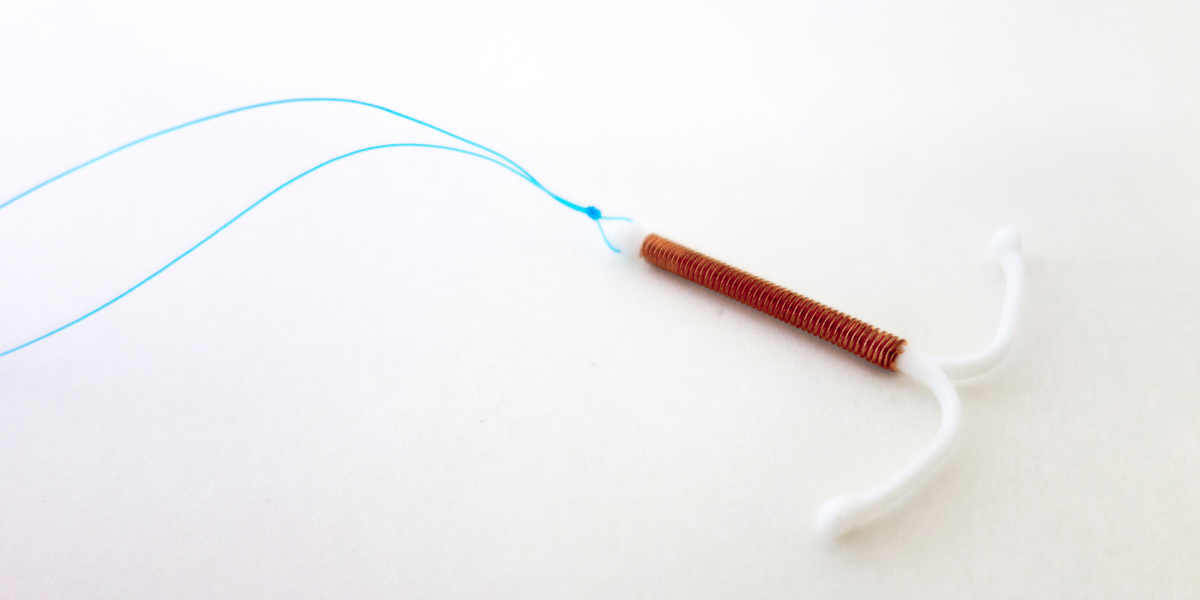
The IUDs available today are small T-shaped devices that are placed in your uterus by your provider. The end of the IUD has strings attached which trail into your vagina for removal when desired. Placement is most commonly done in your physician’s office.
In the past, (the 1970’s), the IUD had a bad reputation for causing pelvic infection, thereby leading to fertility compromise. This increased risk of pelvic infection has been attributed to a particular IUD, called the Dalkon Shield. The Dalkon Shield was different from today’s IUD. The strings of the Dalkon Shield were multifilament, meaning that multiple small strings were coiled together. These strings acted like a conduit or a wick for bacteria to enter the uterine cavity fairly easily.
Today, the IUD continues to have the same configuration but the strings are monofilament. It is still highly advisable for a patient to remain monogamous after IUD insertion and to use condoms to protect from STD transmission But the association with pelvic infection has dramatically decreased.
As mentioned before, the attractiveness of the IUD is effective birth control. Failure rates are less than 1%, which makes IUD one of the most highly effective birth control methods. It allows for spontaneity and yet there is no requirement for daily treatment. Depending on the particular IUD, replacement may not be necessary for either 5 or 10 years.
INSERTION
Insertion may theoretically be performed at any time during the menstrual cycle. However, I attempt to place the IUD at time of menses for two reasons. This ensures that the patient is not pregnant. (If there is a possibility you may be pregnant, YOU MUST INFORM YOUR PHYSICIAN. AN IUD CANNOT BE PLACED IF YOU ARE PREGNANT). The second reason is that the cervix may be slightly more open, allowing for easier insertion.
RISKS
Regardless of contraceptive mechanism, the IUDs all share potential for risk for pelvic infection, (although as noted above this risk is far lower than in the past), expulsion (2-10% in the first year), and uterine perforation. On rare occasions, the IUD strings may retract into the uterine cavity which may make retrieval difficult. If the strings do retract within the uterine cavity, removal may still be accomplished in the office; however, I have had patients require removal with a hysteroscope (a small camera placed into the uterus), under light sedation.
With regards to uterine perforation, the risk of perforation is very small, (approximately 1 per 1,000 insertions). If perforation does occur, damage to nearby organs may be encountered. Perforation may affect the uterus, tubes, ovaries and potentially bowel and bladder or other tissues/organs. Perforation may occur at time of insertion, or shortly thereafter, or may occur years later. With perforation, depending on ultimate location of the IUD, a surgical operation is required to remove the IUD from the abdominal cavity.
Because of this, I prefer to perform IUD insertion under ultrasound guidance for patients that may be more difficult to place. Patients who have never been pregnant or had prior cesarean section deliveries may be better served with ultrasound guided placement. This is because it may be more difficult to pass the IUD through the cervix for these women. HOWEVER, IT IS IMPORTANT TO NOTE THAT EVEN WITH ULTRASOUND GUIDANCE PERFORATION MAY STILL OCCUR. Also it is important to note that insurance may not cover the ultrasound.
TYPES OF IUD
There are two different types of IUDs available. The Paraguard IUD uses copper which inhibits sperm motility, interfering with it’s function and ultimately prevents fertilization. Once placed, it may remain in the uterus for 10 years. The other type of IUD uses a hormone, levonorgesterol, which is a type of progestin. This IUD prevents implantation by thinning the uterine lining and thickening cervical mucus, keeping sperm from entering the uterine cavity. The effectiveness is for 5 years for the Mirena and Kyleena.
COPPER IUD or PARAGUARD IUD
This is a highly effective type of contraception, with a failure rate 0.8%. When placed, a patient may experience heavier menstrual cycles as well as notice increased cramping or discomfort with their cycles. Generally these side effects improve after several months.
MIRENA or KYLEENA IUD
The Mirena IUD is the hormonal IUD which has a failure rate of 0.2%. Because the Mirena thins the endometrial lining, women choosing this form of birth control may also experience a decrease in the duration and heaviness of their menstrual cycles. This is an additional benefit for women who may have heavy menstrual cycles. In fact, I have patients who use the Mirena, not for birth control, but only to make their cycles more manageable.
Mirena is associated with ovarian cysts, and may occur in as many as 17% of patients. These ovarian cysts generally resolve with time, but may be persistent and require further management.
The Kyleena IUD is essentially the “little” Mirena and was designed for young women. This IUD uses the same hormonal properties of the Mirena, but a smaller dose, which in turn allows for a smaller IUD insert and introducer. IUD insertion for the Kyleena requires less cervical dilation and generally a less uncomfortable experience for these patients.